Vaginoplasty / Vaginal Tightening in Bangkok, Thailand
Vaginoplasty is a standard gynecologic surgical procedure that aims to “tighten” a vagina. The vagina has become slack or loose from experience, enlargement due to stressful expansion during childbirth, aging, or outcomes to fixing functional problems, such as urinary incontinence.
Their results can often be loose, weak vaginal muscles. Even after exercise (Kegal exercise), the condition of the vaginal muscles may not improve. The patients will often describe vaginal looseness as a decrease in their ability to attain vaginal orgasms. The result is an immediate decrease in the size of vaginal muscles, resulting in more friction during sexual experiences.
A Good Candidate for a Vaginoplasty
You might be a candidate for a Vaginoplasty if
- You have multiple or prolonged childbirths using forceps or other assisted methods of delivery
- You have vaginal flatulence
- You have a history of constipation and straining with bowel movements
- You are an aging woman
- You have urinary incontinence
- Dyspareunia
Preparation for Vaginoplasty
- Physical examination includes a blood test, chest X-ray, and EKG if the patient is over 40 years old to assess if there is any risk from a heart condition
- Stop smoking for at least two weeks before surgery
- Stop taking anti-inflammatory medications such as Aspirin or ibuprofen for at least two weeks. Also, avoid herbal supplements and vitamins, which may increase bleeding during and after surgery
- The patient will be asked to do a bowel prep before surgery
Vaginoplasty Procedures
Kamol Cosmetic Hospital offers two techniques for a Vaginoplasty as follows;
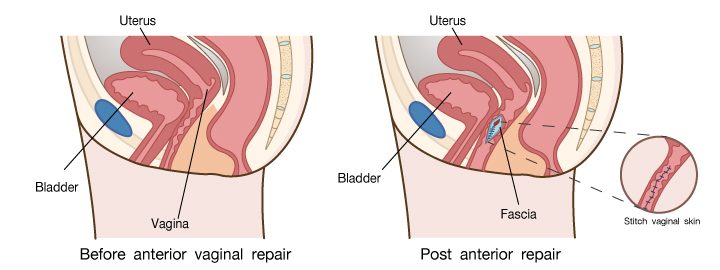
1. Anteria & Posteria vaginal repair (A-P Vaginal Repair) that removes the excessive anterior and posterior vaginal tissues as well as bladder and rectum prolapse, thereby correcting the prolapse and, at the same time, tightening the vagina
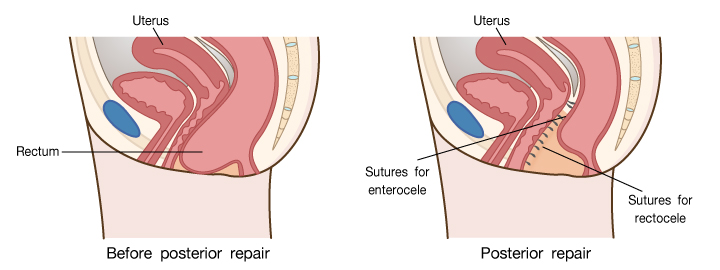
2. Posterior vaginal repair (P-Repair) – removes the excessive posterior vaginal tissues as well as rectum prolapse, thereby correcting the prolapse and, at the same time, tightening the vagina
The procedure is performed in the operating room for approximately 1-2 hours under general anesthesia. The urinary catheter may be inserted to avoid urine retention in the first two days after the operation. When the tension is relieved, the catheter will be removed.
Post-operative Care for Vaginoplasty
- Keep vaginal packing 24 hours after the surgery to stop bleeding
- After surgery, for a few days, you will feel like a passing stool. It causes the sutured posterior vaginal wall. Please take a rest to reduce the symptom and take some medicine for a laxative
- You may take a shower after the catheter is removed, and the surgeon will evaluate your urination after removing the urinary catheter to prevent infection
- Avoid cleaning with water after urinating, but use sanitary wipes to clean the area instead. Water may be used after defecating, followed by a towel to dry the area gently. Do not put anything to wash inside the vagina
- A few days after surgery, recommend a gentle movement to avoid wound disruption
- After the first two weeks, you will have light reddish bleeding out of the vagina; you should use a sanitary napkin for post-operative bleeding. In case of a lot of bleeding, swollen reddish wound, and high fever, don’t hesitate to get in touch with the hospital or meet the doctor immediately
- After the surgery, you can have soft food for a week and then have regular food
- Stop alcohol and smoking for at least two weeks
- You may have abnormal vaginal discharge, a yellowish-green discharge after surgery 6-8 weeks. It may come from vaginal bacteria or incomplete absorption of the suture
- You may have itching or discharge. It can cause a reaction to the suture
Don’t hesitate to contact the hospital or doctor; he will give you some medicine.
Risks and Complications for Vaginoplasty
- Bleeding
- Infection
- Skin and clitoral necrosis
- Rupture of the suture
- Vaginal prolapse
- Fistulas
- Urinary retention
Recovery from Vaginoplasty
- Avoid swimming in the pool, strenuous or heavy activities, and sexual intercourse for 6-8 weeks
- You can have the usual activities after four weeks of the surgery
- Patients can go back to work in one week
- Please follow up with the doctor at every appointment
- The absorbable sutures will dissolve within 6-8 weeks, and if it does not look completely absorbable. The stitches will be removed, and an antihistamine will be used to control the itching
Frequently Asked Questions (FAQs)
What is vaginal tightening or vaginoplasty?
Vaginal tightening, also known as vaginoplasty, is a surgical procedure designed to restore and tighten the vaginal muscles and tissues. This can improve vaginal tone, reduce laxity, and enhance sexual satisfaction.
Think of it like restoring the internal support structure, making things feel firmer and more toned. It isn’t just about aesthetics; it’s about function and confidence.
Why would someone consider vaginal tightening?
Several factors can contribute to vaginal laxity, and reasons for seeking tightening vary:
- Childbirth: Vaginal childbirth can stretch and weaken the vaginal muscles.
- Aging: As we age, the vaginal tissues naturally lose elasticity.
- Genetics: Some women are simply predisposed to having looser vaginal muscles.
- Weight fluctuations: Significant weight gain or loss can affect vaginal tissue.
Many women seek vaginal tightening to improve sexual sensation, address urinary incontinence, or simply regain a sense of confidence and control over their bodies.
Am I a good candidate for vaginal tightening?
An ideal candidate for vaginoplasty is someone who:
- Experiences vaginal laxity: A feeling of looseness or decreased tightness.
- Has realistic expectations: Understanding that the procedure can improve, but not completely restore, vaginal tone.
- Is in good overall health: Fitness for surgery is key to minimizing risks.
- Is not planning future pregnancies: Subsequent vaginal deliveries can reverse the effects of the surgery.
- Has addressed any underlying medical conditions: Such as pelvic floor dysfunction.
What happens during the consultation?
The consultation is an important first step:
- Medical history review: Discuss your overall health and any relevant medical conditions.
- Physical examination: Assessing the degree of vaginal laxity and the overall anatomy.
- Discussion of goals: Understanding your desired outcomes and expectations.
- Explanation of the procedure: Detailing the surgical technique, risks, and benefits.
- Answering your questions: Addressing all of your concerns and ensuring you’re fully informed.
- Psychological Screening: To make sure you are adequately prepared to undergo the procedure.
How do I prepare for vaginal tightening surgery?
Pre-operative preparation is vital for a successful outcome:
- Medical clearance: Undergoing necessary medical tests to ensure you are fit for surgery.
- Stop smoking: Smoking impairs healing and increases the risk of complications.
- Avoid certain medications: Such as blood thinners, which can increase bleeding risk.
- Maintain a healthy diet: Ensuring your body has the nutrients it needs to heal.
- Arrange for transportation and aftercare: Having someone drive you home after surgery and help with household tasks during the initial recovery period.
- Prepare mentally: Understanding what to expect and having a positive mindset can help aid you in your recovery.

